Factors related to depression in patients with dialysis chronic kidney disease: a cross-sectional study
Septa Meriana Lumbantoruan1, Lisandra María Goretti-Sidabutar2
1 Faculty of Nursing. Universitas Pelita Harapan. Tangerang. Indonesia
2 Independent Researcher
https://doi.org/10.37551/S2254-28842025012
Como citar este artículo:
Lumbantoruan SM, Goretti Sidabutar LM. Factors related to depression in patients with dialysis chronic kidney disease:
a cross-sectional study. Enferm Nefrol. 2025;28(2):113-118
Correspondencia:
|
Recepción: 16-03-25
|
ABSTRACT
Introduction: Depression is a frequent yet underrecognized problem among patients with chronic kidney disease undergoing dialysis. The factors related to depression in dialysis patients appear to be varied.
Objetives: To identify clinical and demographic factors related to depression in patients receiving dialysis.
Material and Method: A cross-sectional study was conducted with 50 patients from private hospital in Indonesia. Data collection includes demographic, health-related data, and depression. To identify the depression status, 20 items of Zung Self-Rating Depression Scale were utilized in this study. The data analysis includes univariate, bivariate and multivariate analysis. The dependent variable was analyzed using non-parametric analysis, and to determine the related factors of depression, regression analysis was used in this study.
Results: The average depression score was 31.1 (10.52), indicating no clinical depression in most participants. No demographic variables were associated with depression. Prescribed anti-hypertension and angiotensin-converting enzyme inhibitors were the predictors of depression in patients undergoing dialysis.
Conclusions: Patientes with chronic kidned disease and untreated hypertension experienced higher depression. The use of antihypertensive medications, particularly angiotensin-converting enzyme inhibitors, was associated with lower depression scores in this sample of patients undergoing dialysis.
Keywords: depression; kidney disease; dialysis
RESUMEN
Factores relacionados con la depresión en pacientes con enfermedad renal crónica en diálisis: un estudio transversal
Introducción: La depresión es un problema frecuente, aunque poco reconocido, entre los pacientes con enfermedad renal crónica sometidos a diálisis. Los factores asociados a la depresión en estos pacientes parecen ser diversos.
Objetivos: Identificar los factores clínicos y demográficos relacionados con la depresión en pacientes que reciben diálisis.
Material y Método: Se realizó un estudio transversal con 50 pacientes de un hospital privado de Indonesia. La recogida de datos incluía datos demográficos, datos relacionados con la salud y la depresión. Para identificar el estado de depresión, en este estudio se utilizaron 20 ítems de la escala de depresión autocalificada de Zung. El análisis de los datos incluyó análisis univariante, bivariante y multivariante. La variable dependiente se analizaron mediante un análisis no paramétrico y, para determinar los factores relacionados con la depresión, se utilizó un análisis de regresión.
Resultados: La puntuación media de la escala de depresión fue de 31,1 (10,52), lo que indica ausencia de depresión clínica en la mayoría de los participantes. Ninguna variable demográfica se asoció con la depresión. Los antihipertensivos prescritos y los inhibidores de la enzima convertidora de angiotensina fueron los factores predictivos de la depresión en pacientes con ERC sometidos a diálisis.
Conclusiones: Los pacientes con enfermedad renal crónica e hipertensión no tratada experimentaron mayor depresión. El uso de medicación antihipertensiva, en particular de inhibidores de la enzima conversora de la angiotensina, se asoció a menores puntuaciones de depresión en esta muestra de pacientes en tratamiento con diálisis.
Palabras clave: depresión; enfermedad renal; diálisis.
INTRODUCCIÓN
In 2017, chronic kidney disease (CKD) affected approximately 850 million people worldwide, doubling from 422 million in 20141. Due to this number, CKD is a significant global health issue and contributes to economic burden2. Moreover, it is projected that 2040 CKD will rank among the top five leading causes of mortality worldwide1. Regrettably, the incidence of CKD in Indonesia is documented insufficiently3. Nevertheless, a nationwide survey in 2018 conducted in Indonesia revealed that the prevalence of CKD was 0.5% among a total of 389,093 respondents in that study3. This number is like the prevalence in 2023, accounting for 0.5% of the total population in Indonesia4. Patients with CKD encounter a range of signs and symptoms, both physical and psychological5. Depression is one of the psychological symptoms that are underreported in patients with CKD6. Currently, there is a heightened prevalence of depression among people with CKD. The prevalence varied from 20% to 26% in previous decades7, and the average prevalence has recently spiked to 27.6%6.
Depression in this disease is related to various factors and bidirectional between the depression and the factors8. The related factors are demographics, symptoms of CKD, genetics, and disease-related factors8–10. The consequences of depression in patients with CKD were detrimental, including poor adherence to treatment, increased hospitalization, reduced quality of life, and even mortality due to cardiovascular events6-8. Recent studies about related factors of depression were done in many countries9-10. However, research on this issue was limited in Indonesia. Most of the studies in Indonesia focus on determining the extent of depression and examining the correlation between some variables and depression. Many surveys were also done in general hospitals with low-middle income social statuses. Given the importance of identifying the contributing causes of depression, particularly in the context of private hospitals in Indonesia, it is crucial to conduct this research.
MATERIAL AND METHOD
This was a cross-sectional analytical study, conducted from July to November 2022 in a private hospital in Jakarta, Indonesia. Most of the patients who come to this hospital have middle income family. The ethical permission was obtained from the Ethic Board Universitas Esa Unggul with number 0922-10.011 /DPKE-KEP/FINAL-EA/UEU/X/2022. The population was patients with CKD undergoing dialysis. The inclusion criteria were diagnosed with CKD and undergoing dialysis by the nephrologist, should be adults based on Indonesia law (>18 years old), able to communicate in Bahasa Indonesia, and have stable vital signs. The exclusion criteria were having unstable vital signs and being diagnosed with mental illness. The number of respondents participating in this study was 50 patients. This number is considered an adequate sample size for the regression analysis11.
The data collected in this study included demographic data such as age, gender, marital status, educational background, and occupation. The collected health-related data were CKD duration, dialysis duration, dialysis frequency, type of dialysis, comorbidity, and medication. The Zung Self-Rating Depression Scale (ZDS) was used to determine depression level. This scale was developed in 1965 by Zung and consists of 20 items rated on a Likert scale ranging from 1 to 4 (ZUNG, 1965). This scale demonstrates strong validity and reliability in both its native language and in Bahasa Indonesia. Of the twenty items, ten are negative statements1,3,4,7-10,13,15,19 with a score of 1-4, whereas the other ten items are positive comments. The lowest score achieved by ZDS was 20, while the highest score reached 80. Depression symptoms can be identified if the score is 4012.
Data was analyzed using the Statistical Package for Social Science (SPSS) version 23. Univariate analysis was performed, including frequency and percentage for categorical data, mean, standard deviation, and range for numerical data. The normality of the data was assessed using the Kolmogorov-Smirnov test, Shapiro-Wilk test, and histogram. Due to the abnormality of dependent variables, the bivariate analysis in this study was the Spearmen test, Mann-Whitney test, and Kruskal Wallis test. The statistical method of Ordinary Least Squares regression (OLS) was employed to identify the factors associated with depression. A number 50 sample size is assumed to be enough in regression test13. Moreover, to ensure the results of OLS, a bootstrapped regression analysis was performed in this study14. All alpha levels for inferential analysis were set at 0.05.
RESULTS
Demographic, Health Related Data and Bivariate Analysis
The demographic data and health-related data are shown in table 1 and table 2. In this study, more than half the respondents were younger, with an average age of 54.31 (12.83) and male. Most of them are married, and over 50% have an occupation. From health-related data, all the respondents had dialysis using hemodialysis. Most respondents have comorbidities, such as hypertension, and were prescribed calcium supplements.
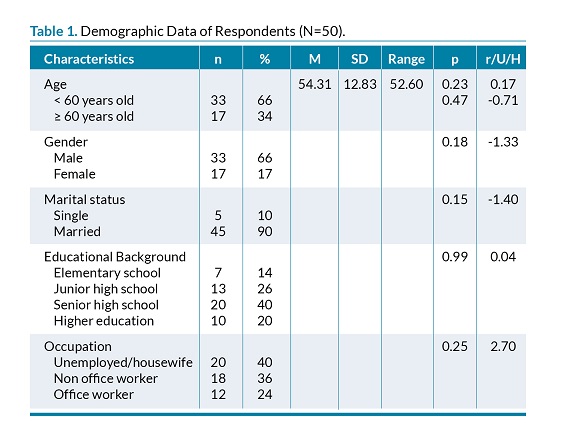
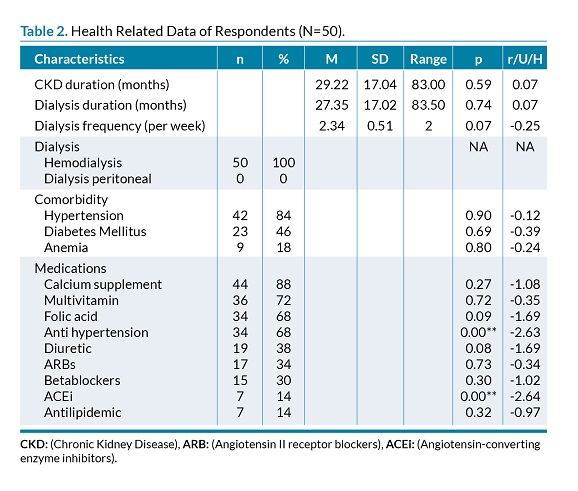
Based on the bivariate analysis, there was no correlation between any of the demographic variables and depression. However, from health-related data, only medicine associated with depression was found, precisely anti-hypertensive drugs and angiotensin-converting-enzyme inhibitors (ACEi). The borderline p-value was influenced by dialysis frequency and diuretic usage. Figure 1 displays the average value of ZDS as 31.1 with a standard deviation of 10.52. Most of the participants indicated a low ZDS score.
Factors Related to Depression
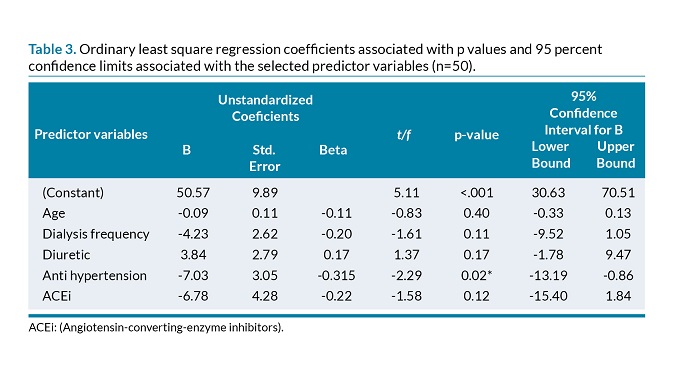
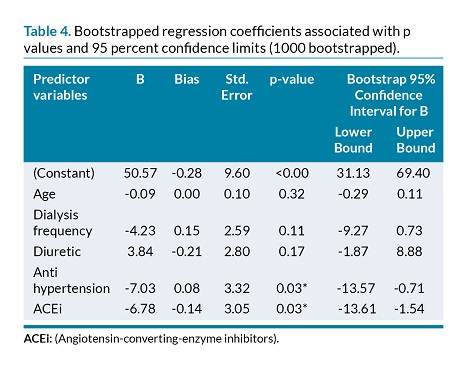
In regression analysis, four independent variables were entered based on the p-value from bivariate analysis. (table 3). The included variables have a p-value<0.1 in the bivariate analysis, including anti-hypertension, ACEi, diuretics, and dialysis frequency. All these variables explain 51.7% of the variance (R2 was 26.7, F 3.2, p<0.05). In OLS analysis, only anti-hypertension is found to be an important factor of depression. Those prescribed anti-hypertension had lower depression scores than those who were not. It is shown that Bootstrap regression was done in this study to confirm the determinant factors of depression. The bootstrap sample included was 1000. The findings support the OLS regression analysis that those who had anti-hypertension tended to have lower depression scores. Moreover, in bootstrap analysis, prescribed ACEi also reduces the score of depression score (table 4).
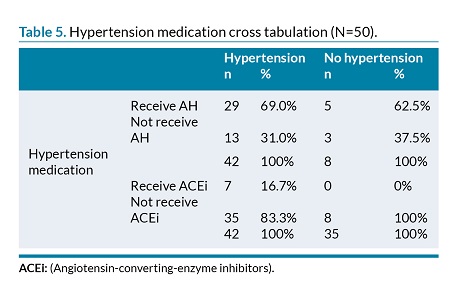
Based on table 5, it shows that not all hypertension respondents are prescribed for anti-hypertension (31%). Most of the respondents (83.3%) also did not receive ACEi.
DISCUSSION
The patients with CKD who underwent dialysis in this study were relatively young compared to a prior study15). The survey by Kovesdy (2022)15 provided an updated analysis of global CKD and reported that CKD was higher in aged people, especially those with an age >70 years old15. Different findings in Indonesia’s health ministry report revealed that younger people, with an average age of 44.3 (15.1) years old, were affected by this condition3. CKD in younger individuals is linked to obesity, hypertension, hyperlipidemia, and diabetes16. Moreover, in this study, most of the respondents had hypertension as comorbidities. The prevalence of hypertension as a comorbidity in Indonesia, as found in a national survey, was only 40.8%3. In comparison, the current finding indicates a greater prevalence. Hypertension, which is a significant risk factor for several conditions such as kidney disease17, is increasing in Indonesia. A substantial proportion of 34.1% of the population was impacted, encompassing both younger individuals and a wide range of other age groups. Indonesia is concerned about this condition and aims to mitigate risk factors, such as hypertension, to lower the prevalence of chronic diseases like CKD18.
In this study, none of demographic data associated with or became the important factor of depression in patients with CKD. This finding was different from previous studies that found a correlation between sociodemographic and marital status associated with depression10. However, age was identified as the important factor influencing depression in studies conducted by Mosleh et al.9,19. The findings of this study indicate that the average age of patients with CKD was lower. However, the increased age was an important factor in depression in previous studies9,19.
This study identified a significant association between anti-hypertension usage and depression, indicating that it is an important factor of depression in patients with CKD. According to the findings, individuals who take anti-hypertension medication exhibited a lower level of depression compared to those who did not receive it. Further investigation has revealed not all patients with CKD with hypertension as the comorbidity receive anti-hypertension. Despite this high prevalence of hypertension among patients with CKD, not all patients with this condition receive appropriate treatment3. Patients with CKD need to maintain their blood pressure to prevent cardiovascular disease. It has been known that uncontrolled blood pressure is linked to cardiovascular mortality in patients with CKD8. Prescribed anti-hypertension might lead to stable blood pressure and stable CKD conditions and make the patients have lower depression scores. As depression in patients with CKD is multifactorial, those with depression can lead to uncontrolled blood pressure, and versa vera8,20.
In this study, the use of ACEi medicine was related to depression and identified as an important factor of depression. However, regression analysis demonstrated no significant influence as a predictor of depression. Following the bootstrap regression analysis, the magnitude of ß was shown was comparable to that of anti-hypertension. This finding suggests that patients who were previously prescribed ACEi had a lower incidence of depression compared to those who were not prescribed ACE inhibitors. ACEi is beneficial in reducing albuminuria and slowing the progression of kidney disease5. Evidence shows that using ACEi therapy controls hypertension in CKD conditions, resulting in better cardiovascular outcomes21. However, despite this benefit, in this current study found that only 16.7% of patients with CKD and hypertension receive ACEi. This finding highlights a gap between theoretical and clinical practical in Indonesia, even in a private hospital. Further study is needed to examine the factors related to the low usage of ACEi in patients with CKD.
Study Limitation
This study has several limitations. First, the rela-tively small sample size may limit the statistical power to detect associations and the generalizability of the findings. Nonetheless, the number of predictors included in the regression model adhered to established methodological recommendation13. Additionally, a bootstrap resampling approach was employed to enhance the robustness of the estimates. Despite these measures, caution is warranted when extrapolating the results beyond populations with similar demographic and clinical characteristics.
CONCLUSION
This study found that patients with chronic kidney disease (CKD) undergoing dialysis exhibited notable levels of depressive symptoms. Among these patients, those with hypertension who were not receiving antihypertensive treatment, particularly ACEi, reported higher depression scores. These findings suggest a potential association between hypertension management and the psychological well-being of individuals with CKD. However, the cross-sectional nature of the study and the limited sample size constrain the interpretation of causal relationships. Further research, ideally through longitudinal or interventional designs, is needed to explore these associations more robustly.
Acknowledge
We thank all the patients who participated in this study.
Conflict of interest
We stated that there is no conflict of interest that was found in this study.
REFERENCES
1. Jager KJ, Kovesdy C, Langham R, Rosenberg M, Jha V, Zoccali C. A single number for advocacy and communication—worldwide more than 850 million individuals have kidney diseases. Nephrology Dialysis Transplantation. 2019;34(11):1803–5.
2. Jha V, Al-Ghamdi SMG, Li G, Wu MS, Stafylas P, Retat L, et al. Global Economic Burden Associated with Chronic Kidney Disease: A Pragmatic Review of Medical Costs for the Inside CKD Research Programme. Adv Ther. 2023 Oct 26;40(10):4405–20.
3. Hustrini NM, Susalit E, Rotmans JI. Prevalence and risk factors for chronic kidney disease in Indonesia: An analysis of the National Basic Health Survey 2018. J Glob Health. 2022 Oct 14;12:04074.
4. Ministry of Health Indonesia. 14 Maret Peringatan Hari Ginjal Sedunia (HGS) [Internet]. 2024; [consultado 2025 Feb 24]. Available from: https://setda.gunungkidulkab.go.id/2024/03/14/14-maret-peringatan-hari-ginjal-sedunia hgs/#:~:text=Menurut%20Kemenkes%20penderita%20penyakit%20ginjal,tahunnya%20karena%20meningkatnya%20jumlah%20penderita
5. Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National Kidney Foundation Practice Guidelines for Chronic Kidney Disease: Evaluation, Classification, and Stratification. Ann Intern Med. 2003;139(2):137–47.
6. Adejumo OA, Edeki IR, Sunday Oyedepo D, Falade J, Yisau OE, Ige OO, et al. Global prevalence of depression in chronic kidney disease: a systematic review and meta-analysis. J Nephrol. 2024;37(9):2455–72.
7. Palapinyo S, Methaneethorn J, Leelakanok N. Association between polypharmacy and depression: a systematic review and meta-analysis. Journal of Pharmacy Practice and Research. 2021;51(4):280–99.
8. Shirazian S. Depression in CKD: Understanding the Mechanisms of Disease. Kidney Int Rep. 2019;4(2):189–90.
9. Qawaqzeh DTA, Masa’deh R, Hamaideh SH, Alkhawaldeh A, ALBashtawy M. Factors affecting the levels of anxiety and depression among patients with end-stage renal disease undergoing hemodialysis. Int Urol Nephrol. 2023;55(11):2887–96.
10. Hawamdeh S, Almari A, Almutairi A, Dator W. Determinants and prevalence of depression in patients with chronic renal disease, and their caregivers. Int J Nephrol Renovasc Dis. 2017;Volume 10:183–9.
11. Wilson Van Voorhis CR, Morgan BL. Understanding Power and Rules of Thumb for Determining Sample Sizes. Tutor Quant Methods Psychol. 2007;3(2):43–50.
12. ZUNG WWK. A Self-Rating Depression Scale. Arch Gen Psychiatry. 1965;12(1):63.
13. Wilson Van Voorhis CR, Morgan BL. Understanding Power and Rules of Thumb for Determining Sample Sizes. Tutor Quant Methods Psychol. 2007;3(2):43–50.
14. Walters SJ, Campbell MJ. The use of bootstrap methods for estimating sample size and analysing health-related quality of life outcomes. Stat Med. 2005;24(7):1075–102.
15. Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl (2011). 2022;12(1):7–11.
16. Kuma A, Kato A. Lifestyle-Related Risk Factors for the Incidence and Progression of Chronic Kidney Disease in the Healthy Young and Middle-Aged Population. Nutrients. 2022;14(18):3787.
17. Fatima S, Mahmood S. Combatting a silent killer - the importance of self-screening of blood pressure from an early age. EXCLI J. 2021;20:1326–7.
18. Riskesdas K. Hasil utama riset kesehata dasar (RISKESDAS). J Phys A Math Theor. 2018;44(8):1–200.
19. Mosleh H, Alenezi M, Al johani S, Alsani A, Fairaq G, Bedaiwi R. Prevalence and Factors of Anxiety and Depression in Chronic Kidney Disease Patients Undergoing Hemodialysis: A Cross-sectional Single-Center Study in Saudi Arabia. Cureus. 2020.
20. D’Oro A, Patel DH, Wass S, Dolber T, Nasir K, Dobre M, et al. Depression and incident cardiovascular disease among patients with chronic kidney disease. International Journal of Cardiology Cardiovascular Risk and Prevention. 2023;18:200199.
21. Zhang Y, He D, Zhang W, Xing Y, Guo Y, Wang F, et al. ACE Inhibitor Benefit to Kidney and Cardiovascular Outcomes for Patients with Non-Dialysis Chronic Kidney Disease Stages 3-5: A Network Meta-Analysis of Randomised Clinical Trials. Drugs. 2020;80(8):797–811.
Este artículo se distribuye bajo una Licencia Creative Commons Atribución–NoComercial 4.0 Internacional.
https://creativecommons.org/licenses/by-nc/4.0/
